I. Liver
The liver is the largest solid organ located in the right upper region of the abdomen, just below the diaphragm. It plays many critical roles, including metabolism, detoxification, production of bile juices, storage of various nutrients, including proteins, and production of clotting factors.
The liver consists of two lobes: the right lobe, which is larger than the left lobe. It has a dual blood supply—one from the intestine and another from the heart.
The liver produces between 700 to 1000 ml of bile juice every day. This bile is emptied into the duodenum through bile ducts or tubes.

Considering its size and location, the liver is affected by a wide range of diseases. Commonly encountered diseases include:
- Infections – Viral, bacterial, and parasitic.
- Trauma.
- Cystic diseases of the liver.
- Benign diseases like hepatic adenomas and hyperplasia.
- Cancers.
1. Drainage of Liver Abscesses
The liver, being the largest solid organ in the body, may develop abscesses or collections of pus within its tissue, leading to various symptoms. These abscesses can be caused by bacterial infections, amoebic infections, or parasitic infections and may be either single or multiple.
Symptoms:
- Abdominal pain.
- Right lower chest pain with pain on deep inspiration.
- High-grade fevers with chills.
- Abdominal bloating.
- Nausea and vomiting.
- Jaundice.
- Occasional history of loose stools a few weeks back.

Diagnosis:
- Clinical examination.
- Blood investigations.
- Ultrasound abdomen and pelvis.
- CT abdomen and pelvis with oral and intravenous contrast.
- MRI.
Treatment:
- Conservative management – Antibiotics and analgesics.
- Percutaneous drainage – Ultrasound or CT guided.
- Surgical management – Laparoscopic / Open drainage.
Laparoscopic Drainage of Abscess:
Surgical drainage may be required for patients who have not improved with conservative treatment or in cases where the abscess bursts, causing pus to disperse throughout the abdomen. In such cases, using small keyholes, the abscess is punctured, pus is drained, and a drain tube is placed for any residual pus to exit.
2. Hydatid Cyst Excision
A hydatid cyst is a zoonotic infection that most commonly occurs in the liver, caused by a parasite, and is commonly seen in people living in proximity to cattle and pets.
Symptoms:
- Abdominal pain.
- Right lower chest pain with pain on deep inspiration.
- Occasional fevers.
- Abdominal bloating.
- Nausea and vomiting.
- Jaundice.

Diagnosis:
- Clinical examination.
- Blood investigations.
- Ultrasound abdomen and pelvis.
- CT abdomen and pelvis with oral and intravenous contrast.
- MRI.
Treatment:
- Percutaneous drainage – Ultrasound or CT guided - PAIR.
- Surgical management – Laparoscopic / Open excision of hydatid cyst / pericystectomy.
Laparoscopic Excision of Hydatid Cyst / Pericystectomy:
Surgical excision will be required in most cases. Surgery is performed after a course of medications (Tab. Albendazole), which is restarted after surgery for a duration of 3-4 weeks. The surgery is conducted using small keyholes, taking adequate precautions to avoid spillage of the cyst contents.
3. Excision of Cystic Tumours / Haemangioma
Cysts, or fluid-filled swellings, and haemangiomas, or tumours arising from blood vessels, are common in the liver. Most of these are detected incidentally during routine health checks or on scans performed for other reasons. Cysts can be congenital and may be multiple. The majority are benign or non-cancerous. Smaller cysts and haemangiomas are usually asymptomatic, while larger ones can cause varied symptoms.
Symptoms:
- Abdominal pain.
- Abdominal fullness / bloating.
- Nausea.
- Vomiting.
- Jaundice.

Diagnosis:
- Clinical examination.
- Blood investigations.
- Ultrasound abdomen and pelvis.
- CT abdomen and pelvis with oral and intravenous contrast (Triple phase).
- MRI.
Treatment:
- Observation and reassurance.
- Embolization in selected cases of haemangioma.
- Surgical management – Laparoscopic / Open deroofing of cysts / excision of haemangiomas.
- Liver transplant in rare cases like polycystic diseases.
Laparoscopic / Open Deroofing of Cysts / Excision of Haemangiomas:
Using small keyholes, large or symptomatic cysts are deroofed, and their contents are suctioned out. In situations where there is communication with the biliary system, additional procedures might be required. Large haemangiomas not amenable to embolization may need excision, which can be performed laparoscopically or, occasionally, via an open technique.
4. Liver Resections: Major / Minor for Cancers and Tumours
Tumours of the liver can be cancerous or non-cancerous. The majority of them are non-cancerous and are incidentally detected on scans. Commonly seen non-cancerous tumours include hepatic adenomas and focal nodular hyperplasia. Treatment of these depends on the symptoms, size, number, and location. Cancerous tumours can arise primarily in the liver (hepatocellular carcinoma) or can be metastatic, having spread from another organ.

Symptoms:
- Abdominal pain.
- Jaundice.
- Fevers.
- Nausea.
- Abdominal fullness.
- Swelling of feet and abdomen.
- Tiredness.
- Loss of weight and appetite.
- Gastrointestinal bleed.
Diagnosis:
- Ultrasound abdomen and pelvis.
- CT scan abdomen and pelvis with intravenous contrast – Triple phase.
- MRI.
- Ultrasound or CT guided biopsy.
- Special blood investigations – CEA, CA-125, CA 19-9, AFP, LDH.
Treatment:
- Observation and reassurance.
- Angio-embolization.
- Trans-arterial chemo-embolization (TACE).
- Trans-arterial radioembolization.
- Radiofrequency ablation.
- Surgery – Laparoscopic / Open liver resection, liver transplant.
Laparoscopic / Open Liver Resection:
In this procedure, a portion of the liver containing the tumour is removed along with an adequate margin. Liver resections can be performed both by laparoscopy and by the regular open technique. The size and location of these tumours aid in choosing the modality of surgery.
II. Biliary Tract
The biliary system, or bile ducts, consists of tubes that carry bile produced in the liver into the small intestine. Initially, these tubes are very small, but they enlarge as they approach the surface of the liver. There are two larger bile ducts: the right and left ducts. These two ducts join to form a single tube known as the common hepatic duct, located near the exit of the liver.
A few centimeters below this confluence is a small, mushroom- or balloon-like out-pouching on the right side called the gallbladder. The gallbladder concentrates bile stored within it, functioning primarily as a storage organ with a capacity of around 50 ml, and has a minimal role in digestion.

The main bile duct, below the level of the gallbladder, is referred to as the common bile duct. This duct joins the pancreatic duct within the duodenum, emptying into it. The opening of these ducts into the small intestine is called the ampulla.
Although the biliary tract is primarily a conduit for bile and digestive juices, it is susceptible to various diseases. Commonly encountered conditions include gallbladder stones, strictures (narrowing), and cancers that may affect the intrahepatic ducts (within the liver tissue) and/or extrahepatic ducts (outside the liver tissue).
1. Gallbladder Stones and Cholecystectomy
The gallbladder, a small balloon-like structure, functions primarily as a storage facility with minimal role in our digestive system. It is susceptible to forming stones and can become infected. Stones are formed due to various reasons and are most frequently seen in females in their fourth decade. The majority of these stones are asymptomatic or silent, with size and number varying significantly.
Symptoms:
- Abdominal pain in the right upper region, which can be mild or severe and may radiate to the back or right shoulder.
- Bloating.
- Fullness after meals.
- Difficulty in taking deep breaths.
- Jaundice.
- Fever.
- Nausea.
- Vomiting.

Diagnosis:
- Ultrasound abdomen and pelvis.
- CT abdomen and pelvis with contrast.
- MRCP.
- Blood investigations – Liver function tests, complete blood counts, coagulation profile.
Treatment:
- Laparoscopic / Open Cholecystectomy.
Laparoscopic / Open Cholecystectomy:
Using multiple (three to four) small keyholes, the gallbladder is removed along with the stones. The laparoscopic approach is preferred and rarely requires the open technique. Being a laparoscopic procedure, it results in less pain, faster recovery, and quicker resumption of routine activities.
2. CBD Explorations for Stones in the Bile Duct
Stones in the bile ducts are frequently encountered, with the majority slipping from the gallbladder and causing blockage of the biliary system, resulting in various symptoms. Both smaller stones or sludge and larger stones can slip into the bile duct, necessitating intervention. Conditions such as narrowing in the bile ducts (strictures) or wide dilatation (choledochal cysts) can also contribute to stone formation within the biliary system.

Symptoms:
- Abdominal pain in the right upper and mid regions below the ribs.
- Nausea.
- Vomiting.
- Jaundice.
- Fever.
- Altered sensorium.
Diagnosis:
- Liver function tests.
- Ultrasound abdomen and pelvis.
- MRI - MRCP.
- Endoscopic ultrasound.
Treatment:
- ERCP – Through endoscope.
- Laparoscopic / Open CBD exploration.
Laparoscopic / Open CBD Exploration:
Surgical removal of bile duct stones is performed when ERCP is not accessible or when ERCP has failed to retrieve the stones. This procedure can be executed through small keyholes or via an open approach. During the surgery, the bile duct is opened along its length, and the stones are extracted under direct vision. Once the stones are removed, a balloon or scope may be used to ensure complete clearance. The opened bile duct is then closed directly or over a tube, which is removed subsequently.
3. Choledochal Cyst Excision
A choledochal cyst is a condition where the bile ducts, both inside and outside the liver, become wider than normal. This widening can occur in a single location or at multiple sites. Based on the location, they are classified into types (I to V), with Type I being the most common. This condition carries a potential risk of harboring cancer, making treatment advisable. Additionally, it can lead to bile stasis and precipitate stone formation.

Symptoms:
- Abdominal pain.
- Fever.
- Nausea.
- Vomiting.
- Jaundice.
- Mass in the abdomen.
- Loss of weight and appetite.
Diagnosis:
- Ultrasound abdomen and pelvis.
- CT abdomen and pelvis with contrast.
- MRI - MRCP.
Treatment:
- Surgical excision – Laparoscopic / Open choledochal cyst excision with hepatico-jejunostomy.
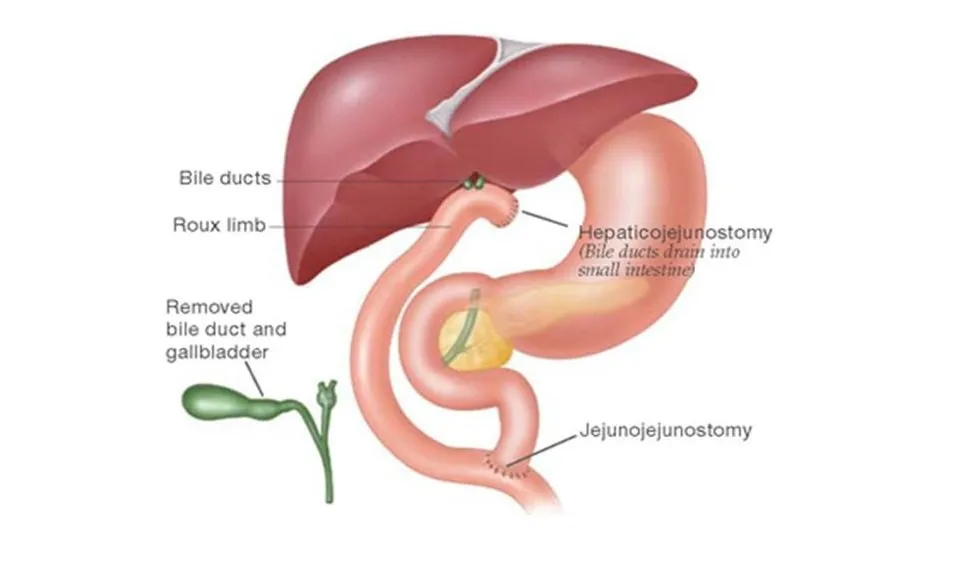
Laparoscopic / Open Choledochal Cyst Excision with Hepatico-jejunostomy:
In this procedure, the cyst is completely removed from its formation to its end. Once excised, the small intestine is divided, and its distal end is brought up and joined to the normal bile duct to ensure smooth bile flow into the intestine, followed by restoration of intestinal continuity. This procedure can be performed using either the traditional open method or the advanced laparoscopic technique with multiple small keyholes.
4. Radical Cholecystectomy for Cancers
Gallbladder cancers are increasingly diagnosed today. The majority of these cancers are identified at presentation, while a smaller percentage are discovered after surgical removal of the gallbladder for stone disease or infection. Surgery remains the mainstay of treatment, and administering chemotherapy prior to surgery has shown benefits in selected cases.
Symptoms:
- Abdominal pain.
- Upper back pain.
- Nausea.
- Vomiting.
- Loss of weight.
- Loss of appetite.
- Jaundice.

Diagnosis:
- CA 19-9.
- CT abdomen and pelvis.
- Endoscopic ultrasound and biopsy.
Treatment:
- Surgery – Laparoscopic / Open radical cholecystectomy.
Laparoscopic / Open Radical Cholecystectomy:
This procedure involves the complete removal of the gallbladder, along with a portion of the liver to which it is attached, through small keyholes or a standard open technique. The lymph nodes surrounding this area are also excised. Occasionally, a portion of the bile duct may also require removal, and reconstruction is performed to restore bile flow.
5. Bile Duct Excision for Tumours and Cancers
Tumours and cancers of the bile tubes are not uncommon. Based on their location, these tumours can present with a variety of symptoms. Tumours may be located within the bile tubes or may compress them from outside.
Symptoms:
- Abdominal pain.
- Fever.
- Jaundice.
- Back ache.
- Loss of weight.
- Loss of appetite.

Diagnosis:
- Ultrasound abdomen and pelvis.
- Endoscopic ultrasound.
- CT abdomen and pelvis with intravenous contrast.
- MRI-MRCP.
Treatment:
- Surgery – Laparoscopic / Open excision +/- liver resection with Hepatico-jejunostomy.
Laparoscopic / Open Excision +/- Liver Resection with Hepatico-jejunostomy:
While laparoscopy can be performed in select cases, open surgery is the standard approach. In this procedure, the affected bile tubes are excised in their entirety along with the surrounding lymph nodes. If the tumour extends into the smaller bile tubes within the liver, a segment of the adjacent liver may also be removed. The gallbladder is also excised as part of the procedure. Once the tumour is removed, bile flow to the intestines is reconstructed and restored.
6. Hepatico-jejunostomy for Strictures
Strictures, or narrowing of the bile tubes, can occur following any previous intervention or surgery on the biliary system. These narrowings are mostly benign or non-cancerous but require a complete evaluation to rule out cancer.
Symptoms:
- Abdominal pain.
- Recurrent fevers.
- Jaundice.
- Chills.
Diagnosis:
- CT abdomen and pelvis with intravenous contrast.
- MRI-MRCP.
- CA 19-9.
Treatment:
- Laparoscopic / Open Hepatico-jejunostomy.
Laparoscopic / Open Hepatico-jejunostomy:
In this procedure, the bile tube with narrowing is completely removed. Once excised, the small intestine is divided, and its distal end is attached to the normal bile tube to ensure smooth bile flow into the intestine. The continuity of the intestine is then restored. This procedure can be performed either through the traditional open technique or using advanced laparoscopic methods with multiple small keyholes.
7. Biliary Bypass for Cancers
Biliary bypass surgeries are performed in cases where complete removal of the disease is not possible due to its advanced nature, as seen in biliary or pancreatic malignancies. This procedure is performed as a palliative measure for selected patients.

Symptoms:
- Abdominal pain.
- Recurrent fevers.
- Jaundice.
- Chills.
Diagnosis:
- CT abdomen and pelvis with intravenous contrast.
- MRI-MRCP.
- CA 19-9.
Treatment:
- Percutaneous biliary bypasses - PTBD.
- Laparoscopic / Open biliary bypass.
Laparoscopic / Open Biliary Bypass:
In this procedure, an obstructed biliary system is provided with an alternate route to empty itself. An accessible portion of the biliary system is connected to the intestine to facilitate this process.
III. Pancreas
Pancreas is a soft gland located behind the stomach. It is a complex organ with a dual role. It has three portions, namely the head, body, and tail. The head of the pancreas lies within the ‘C’ bend of the duodenum to the right of the midline, and its tail lies in close proximity to the spleen in the left upper abdomen.
It has an exocrine function wherein it produces juices for digestion, and it also has a very critical endocrine role, producing hormones like insulin and glucagon required for the maintenance of blood sugars.

Though nestled between other organs, diseases of the pancreas can be severe and life-threatening. It is susceptible to trauma, infections, and malignancies.
Commonly Seen Conditions:
- Acute and Chronic pancreatitis
- Necrotizing or gangrenous pancreatitis
- Cystic lesions of pancreas
- Benign tumours
- Cancers or malignancies
1. Frey's Procedure for Chronic Pancreatitis
Repeated inflammation of the pancreas, due to different reasons, can result in the deposition of calcium in the gland and stones in the ductal system, significantly impairing the function of the gland – production of hormones and digestive juices.
Symptoms:
- Recurrent severe abdomen and back pain
- Vomiting
- Fevers
- Jaundice
- New onset diabetes
- Passing oily stools
- Loss of weight and appetite

Diagnosis:
- Clinical examination
- Blood investigations
- CT abdomen and pelvis (pancreatic protocol) with oral and intravenous contrast
- MRCP
- Endoscopic ultrasound
Treatment:
- Medical management
- Endoscopic management
- Surgical management – Laparoscopic / Open Frey’s head coring and lateral pancreatico-jejunostomy
Laparoscopic / Open Frey’s Head Coring and Lateral Pancreatico-Jejunostomy:
Here, the head portion of the pancreatic gland, which is the cause of all symptoms, is thinned out or removed to a large extent as possible. The duct is opened all along its length, and stones are cleared. Then, an alternate route is created for the pancreatic juices to empty into the intestines (Jejunum). This can be performed through both open and laparoscopic techniques.
2. Cysto-gastrostomy or Jejunostomy for Pseudocysts & Walled Off Pancreatic Necrosis (WOPN)
Pseudocysts occur when, following an attack of pancreatitis, fluid accumulates and becomes localized in the abdomen, typically around the pancreas. These collections may communicate with the main pancreatic duct and can be infected or sterile. Large fluid collections can compress adjacent structures, leading to symptoms.

Symptoms:
- Recurrent abdomen and back pain
- Vomiting
- Intolerance to oral feeds
- Distension or fullness of abdomen
- Fevers
- Jaundice
- New onset diabetes
- Loss of weight and appetite
Diagnosis:
- Clinical examination
- Blood investigations
- CT abdomen and pelvis (pancreatic protocol) with oral and intravenous contrast
- MRCP
- Endoscopic ultrasound
Treatment:
- Endoscopic management
- Surgical management – Laparoscopic / Open Cysto-gastrostomy / Cysto-jejunostomy
Laparoscopic / Open Cysto-gastrostomy / Cysto-jejunostomy:
Based on the location of the fluid collection and the thickness of the wall around it, the technique and type of surgery is determined. Simply put, the cyst fluid is provided an alternate route to empty into the stomach or intestine, using either staplers or sutures.
3. Enucleation of Cystic Lesions
Simple or benign cysts of the pancreas can vary in size and number, from small ones detected during imaging for other conditions to large ones causing symptoms. Cysts may be functional, secreting hormones, or non-functional, and not all cysts require intervention.

Symptoms:
- Recurrent abdomen and back pain
- Vomiting
- Intolerance to oral feeds
- Distension or fullness of abdomen
- Jaundice
- Diarrhea
- Sweating
- Palpitations
- Variations in blood sugars
Diagnosis:
- Clinical examination
- Blood investigations
- CT abdomen and pelvis (pancreatic protocol) with oral and intravenous contrast
- MRCP
- Endoscopic ultrasound
Treatment:
- Endoscopic management
- Surgical management – Laparoscopic / Open enucleation of cysts
Laparoscopic / Open Enucleation of Cysts:
Depending on the location, characteristics, and wall thickness of the cyst, the appropriate intervention is chosen. The cyst is carefully separated from surrounding structures and removed entirely.
4. Necrosectomy for Necrotizing Pancreatitis
Necrosis is the unhealthy or dead portion of tissue, and in this case, we are dealing with necrosis of pancreatic tissue. Necrotizing pancreatitis is commonly seen after a severe attack of pancreatitis or trauma, and it can be either infected or uninfected, involving single or multiple areas around the pancreas.

Symptoms:
- Abdomen and back pain
- Fevers
- Vomiting
- Intolerance to oral feeds
- Distension or fullness of abdomen
- Jaundice
- Variations in blood sugars
- Sepsis
- Shock
Diagnosis:
- Clinical examination
- Blood investigations
- CT abdomen and pelvis (pancreatic protocol) with oral and intravenous contrast
- MRCP
- Endoscopic ultrasound
Treatment:
- Endoscopic management
- Percutaneous drainage
- Surgical management – Laparoscopic / Open necrosectomy
Laparoscopic / Open Necrosectomy:
In patients who do not improve with conservative or other modes of treatment, necrosectomy may be required. The unhealthy, dead tissue is carefully separated and removed, and drains are placed in the cavity to allow for regular post-operative washouts.
5. Distal Pancreatectomy for Tumours and Trauma
Tumours and cancers can develop in any part of the pancreas, including the left or distal portion known as the tail. These tumours vary in type, and treatment depends on the specific type. Additionally, trauma to the abdomen, either blunt or penetrating, can result in pancreatic injury.

Symptoms:
- Tumours: Abdominal pain, back pain, nausea, vomiting, excessive sweating, palpitations, loss of weight and appetite
- Trauma: Abdominal pain, back pain, giddiness, abdominal fullness, fevers, difficulty breathing, vomiting
Investigations:
- Clinical examination
- Blood investigations
- CT scan of the chest, abdomen, and pelvis
Treatment:
- Conservative treatment and follow-up
- Surgery: Laparoscopic / Open Distal Pancreatectomy, +/- splenectomy
Laparoscopic / Open Distal Pancreatectomy, +/- Splenectomy:
Using a laparoscopic technique through small keyholes, the portion of the pancreas containing the tumour is removed with staplers, while preserving the rest of the gland. In some cases, the adjacent spleen may also need to be removed in certain scenarios.
6. Whipple's Procedure for Peri-ampullary Cancers
Cancers affecting the head portion of the pancreas, the lower portion of the bile duct, the ampulla (its opening), or the first portion of the small intestine (duodenum) are gradually increasing in incidence.
Symptoms:
- Jaundice
- Abdominal pain
- Fever
- Loss of weight
- Loss of appetite
- Vomiting
- Abdominal fullness
- Upper and central back pain

Diagnosis:
- Clinical examination
- Blood investigations
- CT scan of the abdomen and pelvis with oral and intravenous contrast
- Endoscopic ultrasound +/- ERCP and biopsy
- +/- PET-CT
Treatment:
- Surgery – Whipple’s procedure
- Chemotherapy
Whipple’s Procedure - Laparoscopic / Open:
The portion containing the cancer is removed along with a portion of the stomach, small intestine, head portion of the pancreas, and bile duct. Using the small intestine (Jejunum), continuity of all organs is restored. In suitable candidates, laparoscopic techniques can be used.









